Renagel
By V. Wilson. New College of Florida. 2018.
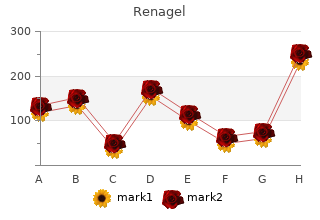
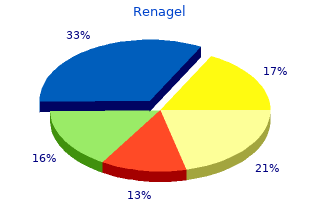
Evaluation of blood count parameters and their association with VTE in the Vienna Cancer and Thrombosis Cohort (N 988 patients with solid tumors only) Hazard ratio** Subhazard ratio†† Variable (95 % CI) P (95% CI) P Hemoglobin (per 1 mg/dL increase) 0 buy renagel 400 mg without a prescription symptoms of gastritis ulcer. Hematology 2014 411 infection by the release of DNA and histones, which subse- and XII. Finally, tissue factor (TF) colocalizes with NETs and quently form a dense local extracellular web that entraps bacteria NET-associated histolytic enzymes such as NE and cathepsin G and fosters the accumulation of microbicidal proteases called degrade its antagonist TF pathway inhibitor directly, thus NETs. Importantly, NETs have been shown to be highly promoting coagulation via the extrinsic pathway. The present mechanistic evidence indicates It is now well established that neutrophil activation occurs not only that neutrophilic NET formation could be the common denominator during infection, but also in inflammatory conditions such as cancer of cancer-associated VTE pathogenesis. However, the current and autoimmunity independent of the presence of infection. In solid enthusiasm about NETs in cancer is not yet supported by clinical cancers, neutrophils represent a dominant cellular species in the local data. Although 8 cancer patients were included in a case-control tumor-surrounding infiltrate. Ideally, a causal relationship between NETosis and VTE in cancer would be established by demonstrating a In terms of thrombosis in malignancy, neutrophilia per se has so far temporal relationship between baseline NET specific biomarkers not been revealed as an independent risk factor for the development and the future occurrence of VTE in a large cancer population of VTE in cancer patients. Nevertheless, the recent discovery of without clinically apparent VTE at baseline. Should this predictive highly thrombogenic NETs as key in vivo propagators of thrombosis relationship emerge in such a study, it is conceivable that NET in a murine cancer model supports the hypothesis that neutrophils biomarkers could be used clinically for the identification of cancer may indeed represent a paramount causal factor for the prothrom- patients at high risk for VTE. Several NETosis candidate biomark- botic state in malignancy. How could neutrophils cause thrombosis in patients with Circulating free DNA is quantifiable with standard laboratory methods,20,21 and may be relatively specific for true NET-derived cancer? Mechanistically, the concept of a “tumor-neutrophil- NETosis-thrombosis axis” appears to emerge from the very DNA. Citrullinated histone 3 appears to be very specific for recent literature on this topic. Tumoral G-CSF overexpression PAD4-dependent neutrophilic chromatin release, but has so far only been measured qualitatively using Western blot. Although the exact processes within the neutrophil fire to the coagulation system in patients with cancer. Further that leads to chromatin degradation and subsequent NET secre- significant developments on this topic may be expected in the near tion are not yet fully elucidated, it appears that the intracellular future when NET biomarkers will be assessed clinically as predic- expression of Peptidylarginine Deiminase 4 (PAD4 or PADI4) is tors of VTE in the cancer setting. The mechanistic relevance of PAD4 for NET-induced Circulating monocytes, which populate tissues as macrophages, thrombogenesis was elegantly shown in a murine inferior vena represent a subgroup of leukocytes that are referred to as the cava stenosis model by Demers et al, in which 9 of 10 PAD4 mononuclear phagocyte system and play a determining role in wild-type mice developed a thrombus within 48 hours after innate and adaptive immunity. Monocytes are the only circulating ligation, whereas only 1 of 11 PAD4-deficient mice did (Figure blood cells that are able to synthesize and express significant 1). TF is a transmembrane receptor and the main in vivo initiator dase (MPO). NETs are then secreted into the extracellular space, of the blood coagulation cascade. A well-described mechanism of where they form a dense prothrombotic web containing citrulli- induction of TF expression on monocytes is the binding of the nated histones, DNA, and histolytic enzymes such as NE, MPO, bacterial endotoxin lipopolysaccharide (LPS) to LPS-binding pro- and cathepsin G. The individual components of this web may tein and CD14, which leads to the activation of the NF- B signaling enter the circulation and exert local and systemic prothrombotic pathway. Specifically, histones increase the generation of throm- creased several-fold by the addition of platelets and granulocytes. A substantial part of Functionally, elevated VWF and thrombin may then lead to the TF activity was not found on the LPS-stimulated monocytes further platelet activation, whereas P-selectin sustains this pro- themselves, but on MPs in the supernatant (which will be discussed cess by attracting more leukocytes and platelets. In a clinical study, Lwaleed et al found have observed in the prospective Vienna CATS that biomarkers that monocyte TF expression was significantly higher in patients and tests such as an elevated in vivo and in vitro thrombin with urological carcinomas than in those with benign tumors and in generation potential, VWF, and P-selectin, represent very strong healthy controls after in vitro stimulation with LPS. Evidence of in vivo NET formation in a murine cancer model.
Comparison of dantrolene sodium and diazepam in the treatment of spasticity purchase renagel 400mg with amex symptoms of gastritis flare up. A comparison of clonidine, cyproheptadine and baclofen in spastic spinal cord injured patients. Effects of a GABA--derivative (BA-34647) on spasticity. Preliminary report of a double-blind cross-over study. Lioresal (baclofen) treatment of spasticity in multiple sclerosis. Evaluation of treatment protocols on minimal to moderate spasticity in multiple sclerosis. An evaluation of baclofen treatment for certain symptoms in patients with spinal cord lesions. The supraspinal anxiolytic effect of baclofen for spasticity reduction. Baclofen in the elderly stroke patient its side-effects and pharmacokinetics. A double-blind comparison of quinine sulphate and placebo in muscle cramps. Baclofen: A team approach to drug evaluation of spasticity in childhood. Skeletal Muscle Relaxants Page 34 of 237 Final Report Update 2 Drug Effectiveness Review Project 95. A double-blind, cross-over trial comparing baclofen with placebo. A controlled trial of baclofen in children with cerebral palsy. The effect of baclofen on the transmission in spinal pathways in spastic multiple sclerosis patients. A controlled, multicenter trial in patients with multiple sclerosis. The use of baclofen in treatment of spasticity in multiple sclerosis. Treatment of spastic cerebral palsied children with sodium dantrolene. Dantrolene sodium in the treatment of spasticity caused by multiple sclerosis or degenerative myelopathies: A double- blind, cross-over study in comparison with placebo. The effect of dantrolene sodium on spasticity in multiple sclerosis. Dantrolene sodium suspension in treatment of spastic cerebral palsy. Objective assessment of spasticity, strength, and function with early exhibition of dantrolene sodium after cerebrovascular accident: a randomized double-blind study. Long-term treatment with dantrolene sodium of stroke patients with spasticity limiting the return of function. Dantrolene sodium in chronic spasticity of varying etiology. Effect of dantrolene sodium on the incidence of seizures in children with spasticity. Spasmolytic properties of dantrolene sodium: Clinical evaluation. Treatment of spasticity in multiple sclerosis with dantrolene. Skeletal Muscle Relaxants Page 35 of 237 Final Report Update 2 Drug Effectiveness Review Project 114. Dantrolene sodium in the treatment of spasticity in chronic spinal cord disease. Antiparetic and antispastic effects induced by tizanidine in patients with spastic paresis. Treatment of spasticity with tizanidine in multiple sclerosis.
Given its excellent efficacy and tolerability renagel 800mg discount chronic gastritis guideline, application of raltegravir is also indicated for treatment-naïve patients. A disadvan- tage is that raltegravir must be taken twice daily, a new formulation is in develop- ment. Minimal pharmacokinetic interaction between the human immun- odeficiency virus nonnucleoside reverse transcriptase inhibitor etravirine and the integrase inhibitor raltegravir in healthy subjects. Simplification of PI + RTV + FTC/TDF to E/C/F/TDF maintains HIV suppres- sion and is well-tolerated. Beck-Engeser GB, Eilat D, Harrer T, Jäck HM, Wabl M. Early onset of autoimmune disease by the retroviral inte- grase inhibitor raltegravir. Transmitted raltegravir resistance in an HIV-1 CRF_AG-infected patient. Dolutegravir versus raltegravir in antiretroviral-experienced, integrase- inhibitor-naive adults with HIV: week 48 results from the randomised, double-blind, non-inferiority SAILING study. Cross-resistance profile of the novel integrase inhibitor Dolutegravir (S/GSK1349572) using clonal viral variants selected in patients failing raltegravir. Dolutegravir in Antiretroviral-Experienced Patients With Raltegravir- and/or Elvitegravir-Resistant HIV-1: 24-Week Results of the Phase III VIKING-3 Study. Inter- and intra-patient variability of raltegravir pharmacokinetics in HIV-1- infected subjects. Once-daily dolutegravir versus darunavir plus ritonavir in antiretroviral- naive adults with HIV-1 infection (FLAMINGO): 48 week results from the randomised open-label phase 3b study. A randomized, double-blind comparison of single-tablet regimen elvite- gravir/cobicistat/emtricitabine/tenofovir DF vs ritonavir-boosted atazanavir plus emtricitabine/tenofovirDF for initial treatment of HIV-1 infection: analysis of week 144 results. Randomized, phase 2 evaluation of two single-tablet regimens elvitegravir/cobici- stat/emtricitabine/tenofovir disoproxil fumarate versus efavirenz/emtricitabine/tenofovir disoproxil fumarate for the initial treatment of HIV infection. Subgroup and resistance analyses of raltegravir for resistant HIV-1 infec- tion. Switch from enfuvirtide to raltegravir in virologically suppressed mul- tidrug-resistant HIV-1-infected patients: a randomized open-label trial. Antiviral activity, pharmacokinetics, and dose response of the HIV-1 inte- grase inhibitor GS-9137 (JTK-303) in treatment-naive and treatment-experienced patients. First report of raltegravir (RAL, MK-0158) use after virologic rebound on elvite- gravir (EVT, GS 9137). Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir diso- proxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomised, double-blind, phase 3, non-inferiority trial. Impact of Y143 HIV-1 integrase mutations on resistance to raltegravir in vitro and in vivo. Safety, tolerability, and pharmacokinetics of the HIV integrase inhibitor dolute- gravir given twice daily with rifampin or once daily with rifabutin: results of a phase 1 study among healthy sub- jects. Overview of antiretroviral agents 105 Dori L, Buonomini AR, Viscione M, Sarmati L, Andreoni M. A case of rhabdomiolysis associated with raltegravir use. A randomized phase 3 study comparing once-daily elvitegravir with twice-daily raltegravir in treatment-experienced subjects with HIV-1 infection: 96-week results. Raltegravir once daily or twice daily in previously untreated patients with HIV-1: a randomised, active-controlled, phase 3 non-inferiority trial. Safety and efficacy of dolutegravir in treatment-experienced subjects with ral- tegravir-resistant HIV type 1 infection: 24-week results of the VIKING Study. Efficacy and safety of raltegravir for treatment of HIV for 5 years in the BENCHMRK studies: final results of two randomised, placebo-controlled trials. Switch to a raltegravir-based regimen versus continuation of a lopinavir-riton- avir-based regimen in stable HIV-infected patients with suppressed viraemia (SWITCHMRK 1+2): two multicen- tre, double-blind, randomised controlled trials. Efficacy and safety of raltegravir in treatment-experienced HIV-1-infected patients switching from enfuvirtide-based regimens: 48 week results of the randomized EASIER ANRS 138 trial.
These events can occur at any time during use and without warning symptoms generic 800 mg renagel otc gastritis diet ������. Elderly patients are at greater risk for serious gastrointestinal events (See WARNINGS). Use of some NSAIDs is associated with an increased incidence of cardiovascular adverse events (such as myocardial infarction, stroke or thrombotic events) which can be fatal. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk • Caution should be exercised in prescribing NSAIDs to any patient with ischemic heart disease (including but NOT limited to acute myocardial infarction, history of myocardial infarction and/or angina), Voltaren SR, Voltaren Rapide, cerebrovascular disease (including but NOT limited to stroke, cerebrovascular accident, transient ischemic attacks and/or amaurosis Ponstan , Mobicox , Naprosyn fugax) and/or congestive heart failure (NYHA II-IV) b E , Naprosyn SR • Use of NSAIDs can promote sodium retention in a dose-dependent manner, through a renal mechanism, which can result in increased blood pressure and/or exacerbation of congestive heart failure. Therefore, caution should be exercised when prescribing NSAIDs • Risk of Gastrointestinal (GI) Adverse Events (see WARNINGS AND PRECAUTIONS–Gastrointestinal) • Use of NSAIDs is associated with an increased incidence of gastrointestinal adverse events (such as peptic/duodenal ulceration, perforation, obstruction and gastrointestinal bleeding). Nonsteroidal antiinflammatory drugs (NSAIDs) 54 of 72 Final Report Update 4 Drug Effectiveness Review Project Appendix C. Glossary This glossary defines terms as they are used in reports produced by the Drug Effectiveness Review Project. Some definitions may vary slightly from other published definitions. Absolute risk: The probability or chance that a person will have a medical event. It is the ratio of the number of people who have a medical event divided by all of the people who could have the event because of their medical condition. Add-on therapy: An additional treatment used in conjunction with the primary or initial treatment. Adherence: Following the course of treatment proscribed by a study protocol. Adverse drug reaction: An adverse effect specifically associated with a drug. Adverse event: A harmful or undesirable outcome that occurs during or after the use of a drug or intervention but is not necessarily caused by it. Adverse effect: An adverse event for which the causal relation between the intervention and the event is at least a reasonable possibility. Active-control trial: A trial comparing a drug in a particular class or group with a drug outside of that class or group. Allocation concealment: The process by which the person determining randomization is blinded to a study participant’s group allocation. Applicability: see External Validity Before-after study: A type nonrandomized study where data are collected before and after patients receive an intervention. Before-after studies can have a single arm or can include a control group. Bias: A systematic error or deviation in results or inferences from the truth. Several types of bias can appear in published trials, including selection bias, performance bias, detection bias, and reporting bias. Bioequivalence: Drug products that contain the same compound in the same amount that meet current official standards, that, when administered to the same person in the same dosage regimen result in equivalent concentrations of drug in blood and tissue. Black box warning: A type of warning that appears on the package insert for prescription drugs that may cause serious adverse effects. It is so named for the black border that usually surrounds the text of the warning. A black box warning means that medical studies indicate that the drug carries a significant risk of serious or even life-threatening adverse effects. The US Food and Drug Administration (FDA) can require a pharmaceutical company to place a black box warning on the labeling of a prescription drug, or in literature describing it. Blinding: A way of making sure that the people involved in a research study — participants, clinicians, or researchers —do not know which participants are assigned to each study group. Blinding usually is used in research studies that compare two or more types of treatment for an illness. Nonsteroidal antiinflammatory drugs (NSAIDs) 55 of 72 Final Report Update 4 Drug Effectiveness Review Project Case series: A study reporting observations on a series of patients receiving the same intervention with no control group.
Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (% renagel 800mg with amex gastritis zunge, adverse Study Design Adverse effects reported n/enrolled n) Comments Malvea Overall incidence: NR NR 1973 United States Side effects possibly related to the use of Fair quality propranolol(# pts): RCT Crossover Mild nausea: 5 Fatigue: 5 Numbness: 1 Heartburn: 1 Heaviness in leg/arm=1 Light-headedness=1 Vomiting=1 Tingling in leg/arm=1 Depressed=1 Mikkelsen Overall adverse effects(# NR 1986 patients): pla=3; Denmark pro=3(NS) Fair quality Adverse events recorded RCT Crossover with: Placebo=slight neurological symptoms, hot flushes, diarrhea Propranolol=fatigue, polyuria, low back pain Beta blockers Page 384 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Pita Migraine (Ad Hoc Committee) at a Concomitant neurological or Propranolol (pro) 160 mg Symptomatic analgesic 1977 frequency of at least 3-4 attacks monthly psychiatric disorders as well as daily treatment (unspecified) Spain and have a history of not responding to diabetes mellitus, asthma or cardiac Placebo (pla) x 2 months; prophylactic therapy disease then crossover Fair quality RCT Crossover Pradalier Suffering from migraine for at least two History of congestive heart failure or Placebo (pla) Usual medication 1989 years with or without aura according to the asthma; heart block; bradycardia (<50 Long-acting propranolol (LA Fair - Poor criteria of the new International Headache beats/min); Raynaud phenomenon; pro) 160 mg daily x 12 weeks RCT Society classification hypertension; resistant to two previously well-followed prophylactic treatments Beta blockers Page 385 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Pita 1) Frequency; 2) duration; 3) severity Mean age=32 Common(#/% patients): NR/NR/9 1977 rated on 3-point scale (e. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Pita NR NR 1977 Spain Fair quality RCT Crossover Pradalier Answers to adverse event LA pro=0 1989 questionnaire at Day 84 pla=1(due to Fair - Poor (LA pro n=22; pla n=19) psoriasis) RCT Cold extremities: LA pro=0; pla=3(15. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Rao Patients with two or more migraine attacks NR Placebo (pla) NR 2000 per week Cyproheptadine (cyp) 4 mg India daily Propranolol (pro) 80 mg daily Fair quality Cyproheptadine 4 mg RCT daily+Propranolol 80 mg daily (cyp+pro) Wideroe Patients diagnosed with cassic or common NR Propranolol (pro) 160 mg Analgesic and 1974 migraine (Ad Hoc Committee, 1962) in daily antimigraine drugs Norway whom the result of open treatment with Placebo (pla) x 3 months, propranolol 160 mg daily as part of a pilot then crossover Fair quality study was rated as "excellent" (e. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Rao Migraine attack frequency, severity Mean NR NR/NR/259 recruited 2000 and duration rated by patient using 5- age=28. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Rao 55 withdrawn/lost to fu Frequency (mean response): pla=1. Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Rao Incidence(# patients): NR 2000 pla=1/69(1. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Poor quality Propranolol Ahuja Suffering from migraine (Ad Hoc Intercurrent illness Propranolol (pro) 120 mg NR 1985 Committee on Headache) at a frequency of daily India > 2 attacks per month in the previous 3 Placebo (pla) x 8 weeks, months then crossover Poor quality RCT Crossover Borgensen (a) Diagnosis of migraine (Ad Hoc Cardiac disease, asthma, diabetes Propranolol (pro) 120 mg NR 1976 Committee on Headache, 1962) mellitus, physical or neurological daily Denmark (b) > 1 migraine attack/week abnormalities Placebo x three months, then (c) Intractability with known prophylactics crossover Poor quality RCT Crossover Beta blockers Page 393 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Poor quality Propranolol Ahuja Severity: rated on 3-point scale Age range of NR NR/NR/26 enrolled 1985 (3=severe; 2=moderate, 17-55 India incapacitating; 1=inconvenient, mild) 46. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Poor quality Propranolol Ahuja NR/NR/NR Attack frequency/8 weeks(mean): pro=8. Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Poor quality Propranolol Ahuja data NR; no significant NR 1985 side effects of propranolol India were observed during the trial period Poor quality RCT Crossover Borgensen NR NR 1976 Denmark Poor quality RCT Crossover Beta blockers Page 396 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Diamond Classic or common migraine Asthma, cardiac disease, diabetes Flexible dosing: Common analgesics, 1976 mellitus or any physical or neurologic Propranolol (pro) 80-160 mg narcotics, ergot United States abnormalities daily medications Placebo (pla) x 4-8 weeks; Poor quality then crossover x 8 weeks RCT Crossover Beta blockers Page 397 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Diamond Severity rated on 3-point scale Average Common migraine: 57 NR/NR/83 1976 (severe/3 headache age=38. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Diamond Incidence(# pts/%): pro=6/83(7. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Fuller Patient record cards n=14 Common NR/NR/27 recruited 1990 Median migraine=9/14(64. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Fuller 14 analyzed Change in headache severity(2 hours post-dose): NR 1990 1-3 point deterioration(# patients): pro=1(7. Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Fuller Propranolol(# patients): NR Study of abortive 1990 Light-headedness=1 treatment of London Stomach pains=1 migraine Sleepiness=1 Poor quality Placebo(# patients): RCT Sleepiness=2 Nausea=2 Dizzness=1 Johnson Incidence: pro=2(8. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Kaniecki 18 to 65 years of age; meeting diagnostic Past trials of valproate or propranolol; Sustained release Symptomatic medication 1997 criteria for migraine without aura as defined failure of greater than 2 adequate trials propranolol (SR pro) 180 mg allowed (unspecified) United States by the IHS; migraine frequency of 2-8 of migraine prophylactic agents; daily times/month, with a maximum of 15 severe medical or psychiatric illness; Divalproex sodium (div) 1500 Poor quality headaches days per month, and a migraine analgesic use of more than 15 days mg daily RCT Crossover history of greater than 1 year per month; presence of alcohol or drug Placebo (pla) Single blind abuse; use of no contraception by women of childbearing potential; unable to complete a headache diary or differentiate various headache types Beta blockers Page 405 of 494 Final Report Update 4 Drug Effectiveness Review Project Evidence Table 16. Placebo controlled trials of beta blockers for migraine Author Year Age Other population Number screened/ Country Method of outcome assessment Gender characteristics eligible/ Study Design and timing of assessment Ethnicity (diagnosis, etc) enrolled Kaniecki Patient diary Mean age NR NR/NR/37 1997 Assessments performed at weeks 4, 81. Placebo controlled trials of beta blockers for migraine Author Number Year withdrawn/ Method of Country lost to fu/ adverse effects Study Design analyzed Outcomes assessment? Placebo controlled trials of beta blockers for migraine Author Withdrawals due Year to adverse events Country (%, adverse Study Design Adverse effects reported n/enrolled n) Comments Kaniecki Adverse event profile for Overall withdrawals 1997 SR propranolol (# events): due to adverse United States nausea=2 events=5(15. Placebo controlled trials of beta blockers for migraine Author Year Allowed other Country Interventions (drug, medications/ Study Design Eligibility criteria Exclusion criteria regimen, duration) interventions Nadelmann Fulfilled diagnostic criteria for classic and/or Migraine other than classic or Propranolol (pro) 80-320 mg Analgesics 1986 common migraine headaches (Ad Hoc common, or other headaches known to daily Tranquilizers Committee on the Classification of be associated with migraine, or if they Placebo (pla) x 30 weeks (6- Ergot Poor quality Headache); had at least four headaches had known contraindications to beta week dose-finding, 24-week Narcotics RCT Crossover per month during a one-month observation blockers double-blind) period Nair History typical of migraine; duration of NR Propranolol (pro) 80 mg daily All patients used 1974 headache of more than one year; attack Placebo (pla) prochlorperazine 15 India rate exceeded 5 or more/month mgms daily throughout the duration of the study.
Does the comparative effectiveness or tolerability and safety of peginterferon alfa-2a plus ribavirin versus peginterferon alfa-2b plus ribavirin vary in patient subgroups defined by demographics (age discount renagel 400 mg with amex gastritis fasting diet, racial groups, gender, genotype, markers of disease severity), use of other medications, or presence of co-morbidities (such as HIV infection)?.................................................... Forest plot on sustained virologic response, dual therapy with pegylated interferon alfa-2a versus dual therapy with non-pegylated interferon alfa-2a or alfa-2b................................................... Forest plot on sustained virologic response, dual therapy with pegylated interferon alfa-2b versus dual therapy with non-pegylated interferon................................................................................ Forest plot on sustained biochemical response, dual therapy with pegylated interferon alfa- 2b versus dual therapy with non-pegylated interferon alfa-2b............................................................... Forest plot on sustained virologic response, dual therapy with pegylated interferon alfa-2a versus pegylated interferon alfa-2a monotherapy................................................................................. Forest plot on withdrawal due to adverse events, dual therapy with pegylated interferon alfa- 2a versus dual therapy with non-pegylated interferon alfa-2a or -2b.................................................... Forest plot on withdrawal due to adverse events, dual therapy with pegylated interferon alfa- 2b versus dual therapy with non-pegylated interferon alfa-2b............................................................... Sustained virologic response rates with different antiviral regimens for hepatitis C virus infection.................................................................................................................................................... Pharmacokinetics, indications and dosing of included drugs................................................... Summary of quality assessment of included published trials................................................. Head-to-head trials of dual therapy with pegylated interferon alfa-2a vs. Characteristics of trials comparing dual therapy with pegylated interferon to dual therapy with non-pegylated interferon........................................................................................................................ Adjusted indirect analysis for sustained virologic response rates.......................................... Trials evaluating efficacy of different doses in regimens of dual therapy with pegylated interferon alfa-2b.................................................................................................................................... Trials evaluating efficacy of different durations of dual therapy with pegylated interferon..... Rates of withdrawals due to adverse events reported in uncontrolled studies..................... Pooled analyses on sustained virologic response rates for genotypes 1, 2, and 3.............. Direct and indirect analyses on sustained virologic response rates for dual therapy with pegylated interferon............................................................................................................................... Quality assessment methods for drug class reviews for the Drug Effectiveness Review Project.................................................................................................................................................... Unpublished trials of pegylated interferons for chronic hepatitis C infection................... Drug Class Review on Pegylated Interferons for Hepatitis C. These organizations selected the topic and had input into the Key Questions for this review. The content and conclusions of the review are entirely determined by the Evidence-based Practice Center researchers. The authors of this report have no financial interest in any company that makes or distributes the products reviewed in this report. Pegylated interferons for hepatitis C Page 4 of 65 Final Report Drug Effectiveness Review Project INTRODUCTION Hepatitis C virus (HCV) is the most common chronic blood borne pathogen in the United States. It is acquired primarily by large or repeated percutaneous exposures to blood, with a history of injection drug use the strongest risk factor. Up to 84% of patients with acute HCV infection develop chronic HCV infection (about 3. Chronic HCV infection has a variable course but can cause cirrhosis, liver failure, and hepatocellular cancer after a number of years.