Lady era
By Q. Jensgar. American Graduate School of International Management. 2018.
Spinal orthotics are generally instituted for curves measuring below 83 Backache and disc disease 60 degrees with definite radiographic evidence of Scheuermann’s disease and can be effective although orthotic compliance is difficult to document cheap lady era 100mg amex pregnancy news, as with scoliosis. Occasionally patients experiencing chronic unremitting pain, who are skeletally mature, and whose curves are 60 degrees or more may warrant surgical stabilization by fusion and instrumentation. From the standpoint of the primary care physician, it is important to be aware of this condition and to establish the correct diagnosis. Backache and disc disease Traditionally, it has been taught that children and adolescents rarely experience back pain and when they do, significant underlying pathology is often present and aggressive investigation is necessary to determine the cause. More recently, however, it has been recognized that back pain is far more common, at least in adolescents, than previously appreciated. Indeed the numbers appear quite similar to those in adults; about 80 percent will have pain that resolves in roughly six weeks and will demonstrate no clear pathologic diagnosis. Accordingly, aggressive investigation into etiology should be undertaken only in selective cases to avoid “medicalizing” transient problems, unnecessarily disturbing parents, identifying radiographic false positives, and unnecessary radiation. It is incumbent on the physician to recognize those children who require a more intense evaluation based upon certain key indicators. As always, a good history and physical examination will rarely mislead the physician. Without question, the most common source of back pain in the adolescent is trauma. In adolescents, mechanical soft tissue strains and bony injury exceed all other causes of back pain combined. Because of the resiliency of the tissues in an adolescent, musculo-ligamentous sprains are far more common than bony injuries. This is directly related to the greater degree of elasticity of the growing spine. There is nothing peculiar to the management of these conditions in childhood as compared with an adult. The remarkable capacity of children to recuperate rather than succumb makes prolonged disability unusual. Magnetic resonance imaging demonstrating intervertebral disc is probably the next most frequent cause of protrusion. Intervertebral disc disease in children is an uncommon cause of back pain but can occur particularly in adolescents. Although the disc can and does degenerate, protrude, sequestrate, and impinge on nerve roots, it does so uncommonly compared with the frequency seen in middle aged adults (Figure 5. On closer scrutiny there seems to be a high incidence of other family members with manifest degenerative disc disease. The history of pre-existent back trauma is much more readily obtained in children than in adults. Involvement of the L5–S1 interspace appears to be the most frequent location for presentation. Magnetic resonance imaging when indicated is the diagnostic test of choice. The indications for conservative and surgical treatment are nearly identical to the adult. It is the rather consistent impression of surgeons caring for this disorder in adolescents that the long-term results of surgical treatment, regardless of type, do not parallel those of the adult, and are routinely poorer. This may in part be due to the fact that these youngsters 85 Backache and disc disease have already demonstrated a genetic weakness within the disc itself, and that they will show other signs of difficulty at other levels later in life. Conservative treatment with physical therapy modalities, non-steroid anti-inflammatories and rest commonly results in resolution of symptoms in 80 to 90 percent of patients within six weeks. Disc space infection in children may occur in this age group but is quite uncommon when compared with the first decade of life. Back pain occurring in concert with idiopathic adolescent scoliosis is a common complaint when carefully scrutinized.
It can be fatal or may lead to rheumatic heart disease cheap lady era 100mg fast delivery menstruation yeast infections, a chronic condition caused by scar- ring and deformity of the heart valves. It is called rheumatic fever because the 2 most common symp- toms are fever and joint pain. Chronic pol- yarthritis perpetuates a gradual destruction of joint tissues and can result in severe deformity and dis- ability. Pathologically, the indicator of rheumatoid arthritis is a positive rheumatoid factor (antibodies that react with immunoglobulin antibodies found in the blood and in the synovium). Interaction between rheumatoid factor and the immunoglobu- lin triggers events that initiate an inflammatory reaction. It typically involves the joints of the fin- gers, hands, wrists, and ankles. As a systemic disease, it can affect the juncture at any articulation (eg, ribs to vertebrae, scapula to clavi- cle). The joints are affected symmetrically, and there is a considerable range of severity. Diseases, Pathologies, and Syndromes Defined 437 sarcoidosis: A systemic disease of unknown origin involving any organ. Sarcoidosis is characterized by granulomatous inflammation present diffusely throughout the body. Secondary sites include skin, eyes, liver, spleen, heart, and small bones in the hands and feet. Symptoms include dyspnea, cough, fever, malaise, weight loss, skin lesions, and erythema nodosum (multiple, tender, nonulcerating nodules). Saturday night palsy: This is a radial nerve compres- sion at the spiral groove of the humerus. Paralysis of upper extremity mus- culature and sensory loss is associated with the level of compression. The mite burrows into the skin and deposits eggs, which hatch, causing the skin erup- tion. It results in low back pain with poten- tial radiation down the back of the lower extremity consistent with the innervation of the sciatic nerve. The curvature of the spine may be to the right (more common in thoracic curves) or left (more common in lumbar curves). Rotation of the vertebral column around its axis occurs and may cause rib cage defor- mity. Infection in the joint caus- es erosion of the joint capsule, leading to arthritic changes in the septic joint. Sick sinus syndrome as a result of degeneration of conductive tissue necessary to maintain normal heart rhythm occurs most often among the elderly. Diseases, Pathologies, and Syndromes Defined 439 somatoform disorder: The presence of physical symp- toms that suggest a medical condition causing sig- nificant impairment in social, occupational, or other areas of functioning. The physical symptoms associated with somatoform disorders are not intentional or under voluntary control. It is a psy- chophysiologic disorder in which emotional prob- lems or conflicts may develop physical symptoms as a means of coping. A defec- tive closure of the bony encasement of the spinal cord (ie, the bony vertebral column is divided into two parts through which the spinal cord and meninges may or may not protrude). If the anom- aly is not visible, the condition is called spina bifida occulta. If there is an external protrusion of the sac- like structure, it is called spina bifida cystica, which is further classified according to the extent of involve- ment (eg, meningocele, meningomyelocele, or myelome-ningocele). Traumatic injury is the most common and is due to a concussion, contusion, or laceration. A concussion is an injury caused by a blow or violent shaking and results in temporary loss of function. Laceration (ie, disruption of tissue) results from complete tran- section of the cord.
Treatment of malignant pain with opioids is now not only ethically acceptable but morally lady era 100 mg line breast cancer 8mm in size, and increasingly, legally, imperative (fig. The To Help and Not to Harm 153 medical community is increasingly viewing the treatment of nonmalignant chronic pain as ethically acceptable and there is growing regulatory acknowl- edgment that this is a legitimate medical practice [2, 13]. The ethical and legal position of treating chronic nonmalignant pain con- tinues to be an area of controversy. The treatment of chronic pain in patients with current SUD or a history of addiction is a much more controversial sub- ject upon which there is much less agreement. Although there are many effective pharmacological, physical, and psychological treatments for chronic pain, a subset of patients with SUD may require opioids for adequate pain relief and acceptable quality of life. There is little scientifically conducted research regarding the risks and benefits of treating chronic pain in patients with sub- stance abuse disorders to guide the practitioner [15, 16]. A small, mostly conceptual body of work on the ethics of treating chronic pain in patients with a current diagnosis and history of a SUD has been pub- lished. A literature search of the databases (Bioethics Line, PsychInfo and Medline) identified 5 articles dealing with the clinical or ethical issues of treat- ing chronic pain in patients with a history of addiction or current SUD and fewer than 10 articles dealing with the ethics of nonmalignant chronic pain treatment [17–20]. One author has called this neglect of the problem of pain in the bioethics literature ‘a legacy of silence’. A Common Language The lack of clear definition of many of the terms involved in this contro- versy contributes to the disagreements. The terms ‘addiction, dependence, toler- ance, and abuse’ have been widely misunderstood and misapplied even among health professionals. The American Academy of Pain Medicine, American Pain Society and American Society of Addiction Medicine produced a consen- sus document containing definitions related to the use of opioids for treating pain. The interpretation of these key terms carries ethical significance. Ethical principles can help frame the clinical import of the key terms employed in scholarly and lay discussions of addiction (table 1). A shared terminology enables all professionals to educate the public about the real nature of addiction and chronic pain diagnoses and their associated pharmacological treatments. The Core Ethical Conflict in Chronic Pain Treatment More than 2000 years ago, Hippocrates succinctly stated the core ethical conflict involved in the treatment of chronic pain in persons with SUD. Ethical acceptability of treating chronic pain Accepted Growing consensus Controversial Malignant pain Chronic nonmalignant pain Chronic nonmalignant pain in addiction use my power to help the sick to the best of my ability and judgment; I will abstain from harming or wronging any man by it’. Ethicists call these two obligations beneficence and nonmaleficence, literally the obligation to do good and not to do harm. Modern codes of ethics continue to regard these ancient principles as two of the physician’s most basic professional obligations. The treatment of chronic pain in any patient accomplishes several recognized goals of medicine: it promotes health and prevents disease; it relieves symptoms of pain and suffering, and it improves functional status or restores previous ability to function. Studies support the contention that treatment of chronic pain with opioids and other psychoactive medications in patients without a history of addiction accomplishes these goals and also may enable patients to return to work and normalize family life [27, 28]. Risk-taking behavior linked to sub- stance abuse as well as the medical complications of addiction may lead to the development of chronic pain conditions necessitating opioid medications for adequate treatment. Between 3 and 16% of chronic pain patients have prob- lems with drug or alcohol abuse [10, 29]. Of 936 patients admitted to a trauma unit in 1988 who had a toxicology screen, 65% were positive for more than one substance. Alcohol-dependent patients are 10 times more likely to become burn victims. Few studies have examined whether the benefits of long-term chronic pain therapy with opioids for chronic pain demonstrated in patients without addiction extend to patients with histories of or active SUD. A 1990 pilot study of methadone maintenance for patients with both chronic pain and substance abuse showed that 3 out of 4 patients remained in treatment for 19–21 months, stopped needle use, and/or markedly decreased substance abuse, and improved functioning despite having a psychopathology serious enough to require psy- chotropic medication. A 2003 study of 44 patients in an integrated 10- week pain management SUD treatment found no difference between patients who continued to take opioids and those who did not during a 12-month follow-up (two thirds of the patients were opioid dependent). Both groups showed reductions in overall medication use while also reporting decreased To Help and Not to Harm 155 pain. Those who continued on opioids were thought to have better functioning, suggesting a potential benefit for chronic pain medication even in patients with SUD.
However purchase 100mg lady era with mastercard menstruation 3 months after delivery, a patient’s goals (and that of those close to him or her) may differ substantially from those of treatment staff and of the funders and referrers who impress their expec- tations on staff. Return to (unsatisfying) work, foregoing compensation due after accidental injury, abstinence from all analgesic and psychotropic drug use, and taking regular exercise are areas where more seems to be ex- pected of pain patients than is achieved by the general (pain-free) popula- tion, and staff and patient may differ on what is a reasonable goal. Although prosaic, it could be that failure to maintain treatment gains lies partly in the choice of goals, and the extent to which they express the patients’ desires and hopes. Further issues in maintenance and generalization may concern the extent to which patients feel “expert” at the end of treatment. Tradi- tional therapeutic relationships can counteract the development of pa- tients’ confidence in their own expertise, rather than respect for staff mem- bers’ knowledge and skills. Although booster sessions are often invoked as the solution, none has shown lasting benefit (Turk, 2001). We still know very little about the processes that undermine treatment gains, given that they are probably as diverse and complex as are patients’ circumstances, and the use of mean data at follow-up (following an implicit model of natural de- cay of treatment gains) is unlikely to disclose any. There remain also hints of the pejorative terminology and patronizing representation of pain patients, explicit in early studies and descriptions of chronic pain populations, and now expressed more in the implication that they have no skills, take no responsibility, and aspire only to recline in the bosom of their enslaved families for their remaining decades. It is notable, but rarely commented on, that although in all other areas of health and ill- 10. PSYCHOLOGICAL INTERVENTIONS AND CHRONIC PAIN 287 ness social support is identified (by theoretical and empirical work) as a po- tent factor promoting health, help provided to pain patients by those around them is often characterized as contributing to disability. A study by Feldman, Downey, and Schaffer-Neitz (1999) is a notable exception, and found social support to have both main and buffering effects against dis- tress associated with pain; an unrelated study by Jamison and Virts (1990) showed good family support (as reported by the patient) to be associated with better outcome of rehabilitation. Most of the work under the rubric of social support comes from patient–spouse interaction and largely corre- lational studies. These were originally thought to support the operant for- mulation, by demonstrating the association of spouse solicitousness and patient disability. However, even these studies and further replications show relationships between patient and spouse behavior to be mediated by gender, state of the relationship, and mood: The picture is substantially more complicated than suggested by the dominant study paradigms and measures of the 1980s and 1990s (Newton-John & Williams, 2000). FAMILY AND MARITAL THERAPY Background and Description Family and or marital therapy is also used as an adjunct to the treatment of chronic pain in adults, and more directly in relation to pain and related be- havior in children and adolescents, but much less is written regarding the topic (Kerns & Payne, 1996). The interest in treating the family of the chronic pain patient comes from recognition that not only the patient but also the spouse and other family members suffer the impact of pain. All family members are likely to experience reductions in leisure activities, changes in responsibilities and roles, and changes in how emotions are ex- pressed (Turk et al. Some therapists take a traditional family systems approach and focus on how the family may or may not be using or developing resources and capacities to meet the de- mands of chronic pain (Patterson & Garwick, 1994). With this approach, the therapist attempts to restore a comfortable balance in the family system in light of the pain (Moore & Chaney, 1985). Alternatively, a family therapist may take an operant approach as described earlier. Fordyce (1976) in his early writings recommended that in some cases patients be refused treat- ment without spouse involvement, although today this would be regarded as ethically unacceptable. In this approach, the focus is on how pain behav- iors are maintained by contingent social reinforcement (Fordyce, 1976) and draws on evidence showing that pain behavior can be influenced by 288 HADJISTAVROPOULOS AND WILLIAMS spousal reactions to pain (e. Family mem- bers are encouraged to withhold pain-contingent attention and instead rein- force well behaviors. Central to this approach is the belief that family members help patients understand the painful condition, and make judgments about the family and patient’s ability to meet the challenge of the condition. The family develops beliefs about pain, disability, and emotional responses, which in turn influence how the patient and family members deal with the challenges of chronic pain (Kerns & Weiss, 1994). With this treatment approach, family members and the patient are encouraged to identify and develop strategies for cop- ing with the effects of pain (Moore & Chaney, 1985), and to express the pa- tient’s needs directly and verbally, rather than indirectly and through pain behaviors—hence, the teaching of assertion skills and the recognition of the need to negotiate for help and exchange of favors, rather than one-way helping, which ultimately benefits neither patient nor family caregivers. Evidence Despite strong clinical assumptions that the family is important in deter- mining response to chronic pain (e. Moore and Chaney (1985) evaluated the efficacy of out- patient group treatment of chronic pain and the effect of the spouse in- volvement in treatment; they randomly assigned patients to couples group treatment, patient-only group treatment, or waiting list control. Both groups showed improvement on several measures, including pain behavior and functioning, marital satisfaction, and health care utilization.
As the enteral feeding volume is increased and absorbed by the patient buy generic lady era 100mg on line women's health gov publications our fact sheet birth control methods, intravenous fluid are diminished at the same rate, so that the total amount of resuscitation needs are met as a mixture of IV fluids and enteral feeding. By 48 h, most of the fluid replacement should be provided via the enteral route. The response to fluid administration and physiological tolerance of the patient is most important. TABLE 7 Resuscitation Formulas for Pediatric and Adult Patients Pediatric Patients First 24 h: 5000 ml/m2 BSA burned/day 2000 ml/m2 BSA total/day of Ringer’s lactate (give half in first 8 h and the second half in the following 16 h) Subsequent 24 h: 3750 ml/m2 BSA burned/day 1500 ml/m2 BSA total/day (to maintain urine output of 1ml/kg/h) Adult Patients First 24 h: 3 ml/kg/% BSA burned of Ringer’s lactate (give half in first 8 h and the second half in the following 16 h) Subsequent 24 h: 1 ml/kg/% burn daily (to maintain urine output of 0. Fluid resuscitation should be started according to the fluid resuscitation formula. Fluid administration needs then to be tailored to the response of the patient based on urine output in a stable, lucid cooperative patient. The ideal is to reach the smallest fluid administration rate that provides an adequate urine output. The appropriate resus- citation regimen administers the minimal amount of fluid necessary for mainte- nance of vital organ perfusion. Inadequate resuscitation can cause further insult to pulmonary, renal, and mesenteric vascular beds. It will also increase wound edema and thereby dermal ischemia, producing increased depth and extent of cutaneous damage. Fluid requirements in patients with electrical injuries are often greater than those in patients with thermal injury. The main threat in the initial period is the development of acute tubular necrosis and acute renal insufficiency related to the precipitation of myoglobulin and other cellular products. A common finding in patients with electrical injuries is myoglobinuria, manifested as highly concen- trated and pigmented urine. The goal under these circumstances is to maintain a urine output of 1–2 ml/kg/h until the urine clears. In nonresponding patients, alkalization of the urine and the use of osmotic agents may prevent death. The use of colloid solutions for acute burn resuscitation remains debated. Development of hypoproteinemia in the early resuscitation period increases edema in nonburned tissues. In the absence of inhalation injury, however, lung water content does not increase. Early infusion of colloid solutions may decrease overall fluid requirements in the initial resuscitation period and reduce nonburn edema. However, injudicious use of colloid infusion may cause iatrogenic pulmo- nary edema, increasing pulmonary complications and mortality. The current rec- ommendation is to add 25% albumin solution to maintain serum albumin 2. Albumin solution 5% should be used instead of 25% solution in unstable patients with hypovolemia. Hypotension is a late finding in burn shock; therefore, pulse rate is much more sensitive than blood pressure. Normal senso- rium, core temperature, and adequate peripheral capillary refill are additional clinical indicators of adequate organ perfusion. Fluid shifts are rapid during the acute resuscitation period (24–72 h), and serial determinations of hematocrit, serum electrolytes, osmolality, calcium, glucose, and albumin can help to direct appropriate fluid replacement. Although overresuscitation is usually easy to detect, based on increasing edema and high urine output; underresuscitation may be much more difficult to diagnose and categorize. Persistent metabolic acidosis on measurement 28 Barret FIGURE 10 Approach to the nonresponding patient. Resuscitation fluids must be reviewed and corrected (including fluid boluses) before any other further action is taken.
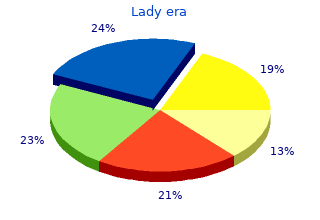
9 of 10 - Review by Q. Jensgar
Votes: 205 votes
Total customer reviews: 205